ID: PMRREP24595| 190 Pages | 22 Jan 2026 | Format: PDF, Excel, PPT* | Healthcare

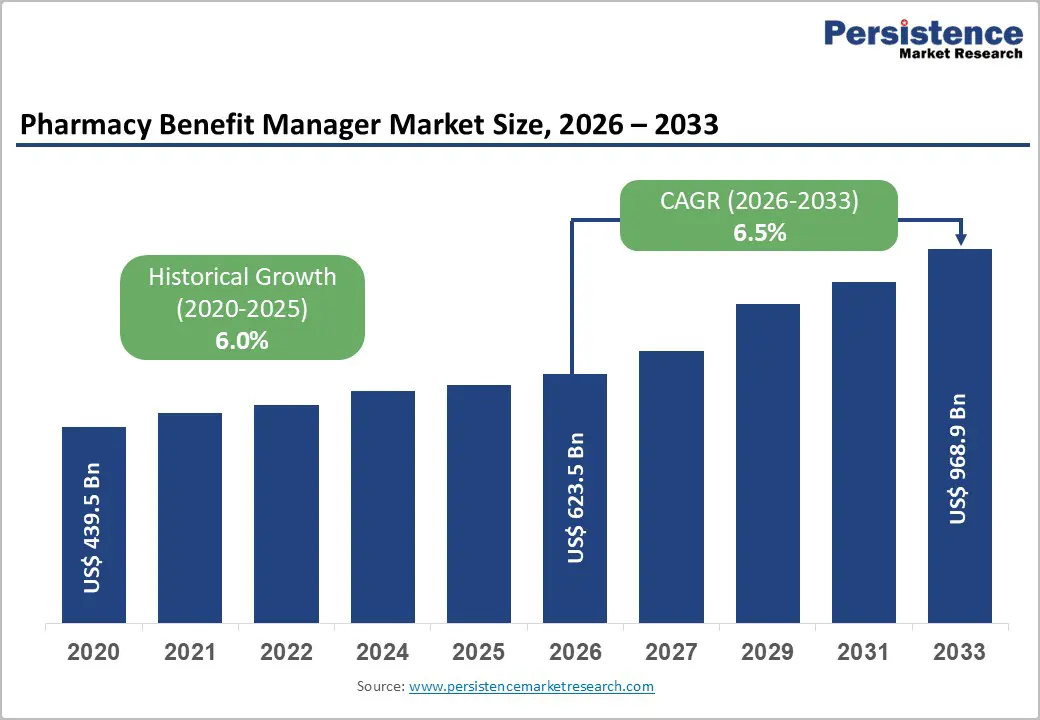
The global pharmacy benefit manager market size is expected to be valued at US$ 623.5 billion in 2026 and projected to reach US$ 968.9 billion by 2033, growing at a CAGR of 6.5% between 2026 and 2033.
The Pharmacy Benefit Manager market is expanding due to escalating prescription drug costs, with U.S. spending hitting $576.9 billion in 2021, according to CMS data. Growing prevalence of chronic diseases and increasing demand for specialty medications are driving the need for efficient management of pharmacy benefits.
PBMs play a key role in cost containment, formulary management, and optimizing patient access. Adoption of value-based care models further strengthens their position by aligning drug utilization with clinical outcomes. Advances in technology, data analytics, and digital platforms are enhancing PBM capabilities, supporting operational efficiency, reducing overall healthcare expenditures, and driving market growth globally.
| Key Insights | Details |
|---|---|
| Pharmacy Benefit Manager Market Size (2026E) | US$ 623.5 Bn |
| Market Value Forecast (2033F) | US$ 968.9 Bn |
| Projected Growth (CAGR 2026 to 2033) | 6.5% |
| Historical Market Growth (CAGR 2020 to 2025) | 6.0% |
The global rise in chronic disorders is significantly increasing the demand for prescription treatments, particularly high-cost branded medications produced by large pharmaceutical companies. This trend has led to a substantial surge in pharmaceutical spending in recent years. In the United States, medicine prices rose by 4% in 2021, breaking previous patterns of moderate increases, while individual prescription drug prices increased by 5%, according to SingleCare Administrators. The escalating cost of medications, combined with the growing number of prescriptions for chronic conditions such as cardiovascular disease, diabetes, and chronic respiratory illnesses, is adding to the overall healthcare burden.
The rising pharmaceutical expenses are prompting healthcare stakeholders to seek solutions that can manage costs effectively. Pharmacy Benefit Managers (PBMs) have emerged as critical players in controlling drug spending by negotiating prices, managing formularies, and optimizing patient access to medications. With approximately 4 billion prescriptions filled annually in the U.S., the adoption of PBMs is becoming increasingly necessary to streamline drug utilization, reduce costs, and improve efficiency in pharmaceutical supply chains. This combination of higher drug prices and increased prescription volumes is expected to drive substantial growth in the global PBM market over the forecast period.
Despite their role in controlling drug costs, Pharmacy Benefit Managers face growing scrutiny over transparency in their business models. PBMs often do not disclose revenue sources to pharmaceutical manufacturers, retail pharmacies, or insurance providers. A significant portion of overall spending on brand-name drugs flows to PBMs rather than directly benefiting drug makers, creating concerns among industry stakeholders. According to Berkeley Research Group, over 50% of brand drug spending is directed through the supply chain, including PBMs, which reduces profit margins for both insurers and manufacturers.
This lack of clarity has led to hesitation among insurance companies to partner with PBMs. Some insurers have completely avoided PBM arrangements, while others remain cautious due to perceived conflicts of interest and limited visibility into cost allocation. As a result, adoption rates of PBM services are being slowed, particularly in regions where regulatory oversight and stakeholder accountability are stringent. This growing concern regarding transparency and its potential impact on trust and profitability is expected to restrain the growth of the global Pharmacy Benefit Manager market during the forecast period.
The integration of advanced technologies such as machine learning (ML) and artificial intelligence (AI) presents significant growth opportunities for the Pharmacy Benefit Manager market. Traditional PBM workflows are increasingly being augmented with AI-driven platforms that streamline claim processing, optimize supply chain management, and reduce human error. For example, leading U.S.-based PBM CAPITAL RX employs AI and ML algorithms to accelerate claim approvals and enhance operational efficiency. These technologies enable PBMs to manage a large volume of prescriptions across retail pharmacies, insurance networks, and healthcare providers, improving coverage accuracy while minimizing delays.
Furthermore, AI and ML adoption enhances cost-containment capabilities and improves the overall patient experience by enabling faster mail-order pharmacy services, predictive analytics for drug utilization, and personalized medication management. The ability to process complex datasets efficiently allows PBMs to negotiate better pricing and optimize formularies, benefiting both payers and patients. As healthcare systems increasingly focus on digital transformation and value-based care, the deployment of AI and ML solutions offers PBMs an opportunity to expand service offerings, reduce operational costs, and increase market penetration. This technological shift is poised to drive long-term growth and competitiveness in the global PBM market.
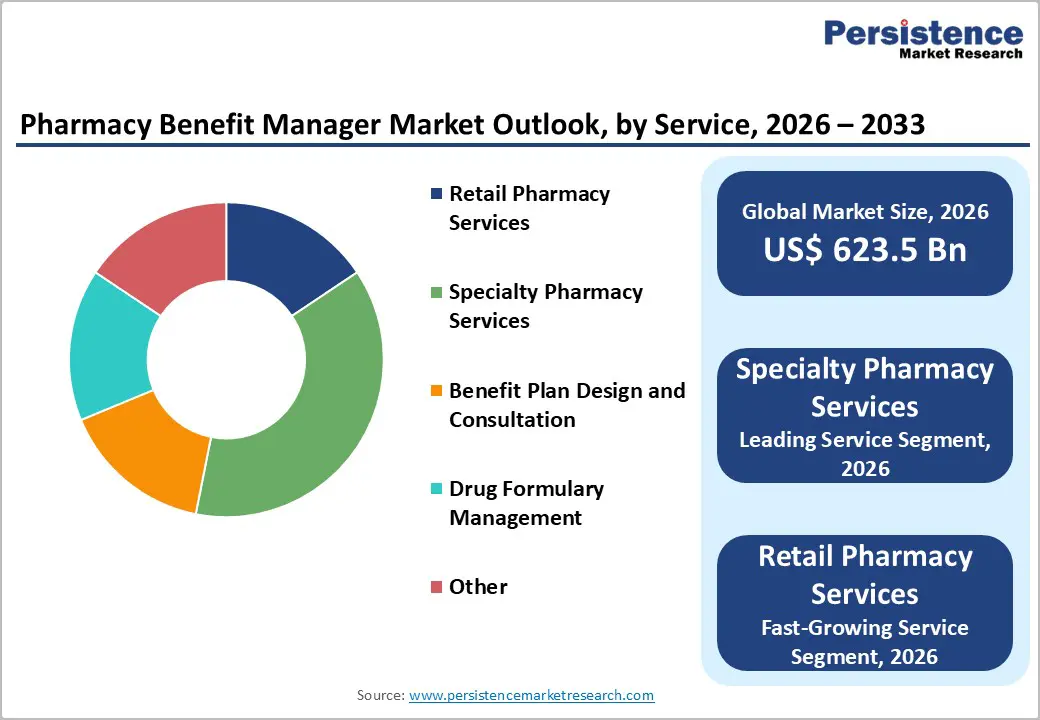
Specialty pharmacy services are projected to lead the Pharmacy Benefit Manager market with an estimated 36% share in 2026, driven by their ability to manage complex and high-cost biologic medications. While specialty drugs account for only 1–2% of prescription volumes, they represent nearly 50% of overall drug spending in the United States, highlighting the critical role of these services in controlling costs. Specialty PBMs ensure proper cold-chain logistics, adherence support, and patient counseling for approximately 40 million patients, mitigating risks associated with biologic therapies. Their focus on patient outcomes and clinical management enhances therapy effectiveness, while real-world evidence helps optimize formulary decisions. According to the Federal Trade Commission (FTC), PBM networks account for 66% of total revenue within the sector, reflecting the widespread adoption and influence of specialty pharmacy services. The combination of operational efficiency, adherence programs, and data-driven formulary management solidifies specialty pharmacy services as the dominant service segment within the PBM landscape.
Health insurance companies are expected to hold roughly 50% of the market share in 2026, driven by their vertically integrated Pharmacy Benefit Manager models that streamline claims processing, formulary management, and rebate optimization. These integrated PBMs serve around 200 million insured lives, leveraging scale to negotiate pricing and manage specialty and traditional medications effectively. Vertically aligned providers such as OptumRx capture about 22% of the market share, benefiting from close coordination with parent health plans and data insights that optimize formulary placement and rebate strategies across commercial, Medicare, and Medicaid programs. The reliance of CMS Medicare Part D on PBMs further reinforces the dominance of health insurance companies in the market, enabling large-scale adoption of cost-containment strategies. By integrating clinical management, utilization review, and advanced analytics, insurance-led PBMs can efficiently control drug spending, improve patient adherence, and enhance operational efficiency. Their widespread reach, financial strength, and ability to influence formulary decisions make health insurance companies the leading service provider segment in the PBM market.
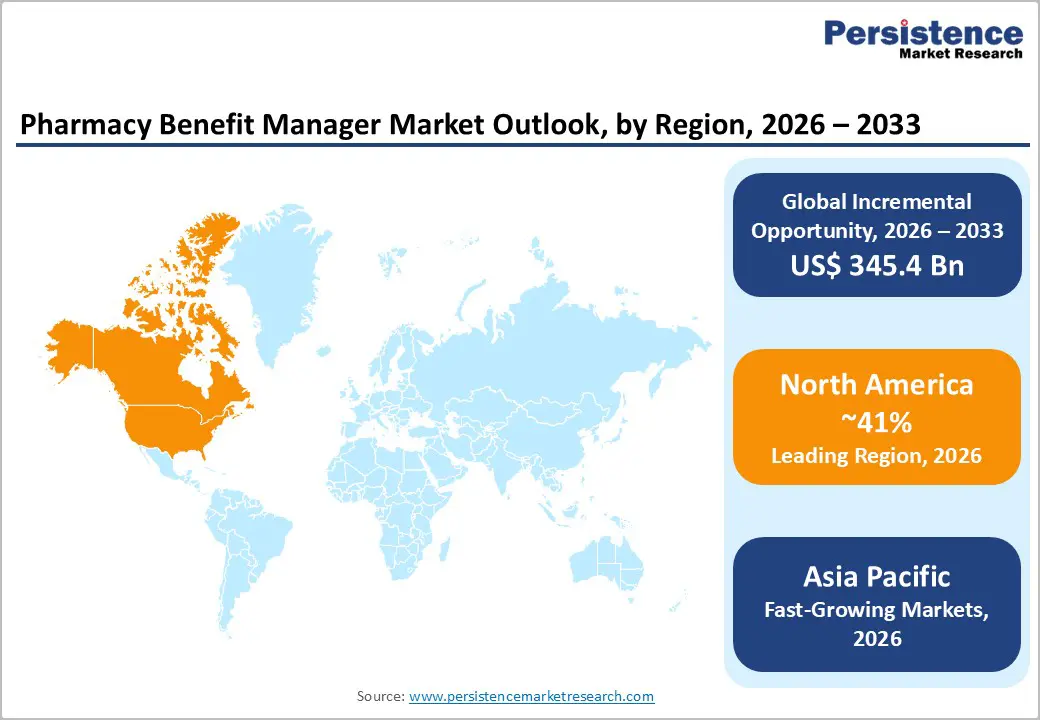
North America, led by the United States, dominates the global Pharmacy Benefit Manager (PBM) market, accounting for approximately 66.5% of total market share. The region benefits from a well-established healthcare ecosystem, including major insurance providers, pharmaceutical manufacturers, retail pharmacy chains, and PBM service companies. Rising adoption of health insurance policies is a key growth driver, as over half of the U.S. population is affected by one or more chronic conditions, increasing demand for prescription medications and cost management solutions. The escalating cost of healthcare further reinforces the need for PBMs to negotiate drug prices, optimize formularies, and manage specialty drug programs efficiently. According to the Centers for Medicare and Medicaid Services (CMS), total healthcare spending in the U.S. increased by 9.8% in 2020, highlighting the growing financial burden on patients and payers. Favorable reimbursement policies and reliance on insurance coverage for treatment also support PBM adoption. Combined, these factors contribute to the steady expansion of the PBM market across North America, particularly in hospital networks, retail pharmacies, and integrated insurance models.
The Asia Pacific Pharmacy Benefit Manager market is emerging as the fastest-growing regional segment, driven by rising chronic disease prevalence, increasing healthcare expenditure, and expanding health insurance coverage across countries such as China, India, Japan, and Southeast Asia. Rapid urbanization, lifestyle changes, and an aging population have contributed to higher incidence of chronic conditions, boosting demand for prescription medications and specialty drugs. Governments in the region are introducing policies to improve drug affordability and access, including reimbursement frameworks, public insurance schemes, and digital health initiatives, which create opportunities for PBM adoption. The growing presence of multinational PBM providers and local partnerships helps facilitate formulary management, claims processing, and cost-containment solutions in hospitals, clinics, and retail pharmacies. Additionally, technological advancements such as integrated pharmacy management platforms and point-of-care solutions enhance operational efficiency and patient adherence. Rising awareness of cost management among payers and patients, coupled with increasing investments in healthcare infrastructure, is expected to drive sustained PBM market growth throughout the Asia Pacific region during the forecast period.
The global Pharmacy Benefit Manager (PBM) market is highly competitive, with leading players leveraging multiple strategies to maintain and expand their market presence. Companies are investing in research and development, launching innovative products, and adopting advanced technologies to enhance service efficiency and patient outcomes. Strategic collaborations, partnerships, and acquisitions enable PBMs to enter new geographic regions and expand their service portfolios. Marketing initiatives and operational improvements help strengthen brand recognition and customer loyalty. This combination of innovation, strategic expansion, and technological integration allows key market players to consolidate their positions while capturing growth opportunities in both developed and emerging markets.?
The global pharmacy benefit manager market is expected to reach US$ 623.5 billion in 2026.
Increasing prices of branded and specialty medications are driving demand for PBMs to manage costs.
North America leads with 41% share in 2025, driven by CMS and high spend.
Integration of Artificial Intelligence (AI) and Machine Learning (ML) can streamline claims processing, optimize formulary management, reduce errors, and improve patient adherence.
Leaders include Express Scripts Holding Company, CVS Health Corporation, DST Systems, Inc., Rite Aid Corp., and ProCare Rx.
| Report Attribute | Details |
|---|---|
|
Historical Data/Actuals |
2020 - 2025 |
|
Forecast Period |
2026 - 2033 |
|
Market Analysis |
Value: US$ Bn Volume (Units) If Applicable |
|
Geographical Coverage |
|
|
Segmental Coverage |
|
|
Competitive Analysis |
|
|
Report Highlights |
|
Service
Service Provider
Regions
Delivery Timelines
For more information on this report and its delivery timelines please get in touch with our sales team.
About Author