ID: PMRREP35536| 200 Pages | 31 Jul 2025 | Format: PDF, Excel, PPT* | Healthcare

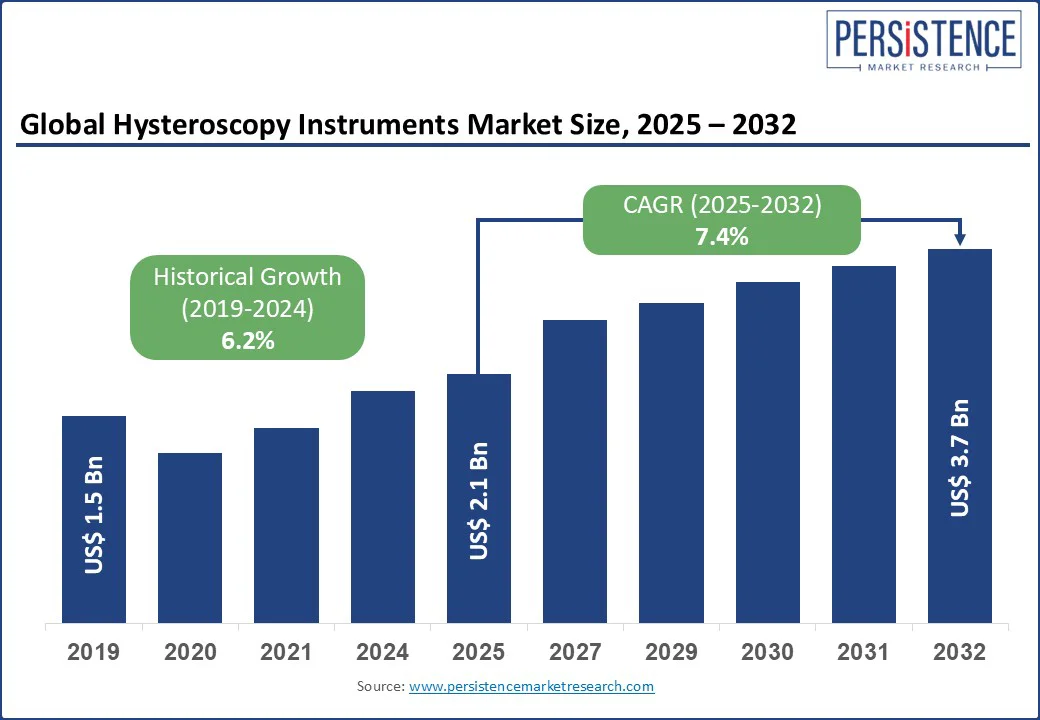
The hysteroscopy instruments market size is likely to be valued at US$ 2.1 Bn in 2025 and is estimated to reach US$ 3.7 Bn in 2032, growing at a CAGR of 7.4% during the forecast period 2025-2032. Procedural miniaturization, evolving outpatient care models, and rising gynecological case volumes encourages the demand for clinical instruments. As healthcare providers shift toward office-based diagnostic and operative interventions, demand is rising for compact tools. Multifunctional hysteroscopy instruments are being developed to help reduce patient recovery time and improve clinical throughput. Leading players are also introducing integrated hysteroscopic platforms, novel fluid management systems, and disposable instrument kits for ambulatory settings.
Key Industry Highlights
|
Global Market Attribute |
Key Insights |
|
Hysteroscopy Instruments Market Size (2025E) |
US$ 2.1 Bn |
|
Market Value Forecast (2032F) |
US$ 3.7 Bn |
|
Projected Growth (CAGR 2025 to 2032) |
7.4% |
|
Historical Market Growth (CAGR 2019 to 2024) |
6.2% |
Increasing prevalence of gynecological disorders, including Abnormal Uterine Bleeding (AUB), uterine fibroids, and endometriosis, is pushing the hysteroscopy instruments market growth. The International Federation of Gynecology and Obstetrics (FIGO), for example, predicts that about 15 to 25% of women of reproductive age experience AUB. Hysteroscopy has become the gold-standard approach for analyzing endometrial causes, such as polyps or submucosal fibroids. It has resulted in surging adoption of hysteroscopic instruments in both diagnostic centers and OB/GYN clinics, primarily those offering one-stop fertility check-ups.
Rising surgical treatment rate of uterine fibroids has further pushed the use of operative hysteroscopic tools, including resectoscopes and morcellators. According to the U.S. Department of Health and Human Services, approximately 20 to 80% of women develop fibroids by the time they reach the age of 50. The surge in early-stage detection of endometrial or cervical abnormalities through routine screenings and HPV testing is further pushing diagnostic hysteroscopy volumes.
The risks of complications such as uterine perforation, fluid overload, and air embolism continue to hamper the full-scale adoption of hysteroscopy instruments. It is evident in low-resource settings and among less experienced operators. Uterine perforation, while relatively rare, remains a key concern during operative hysteroscopy, mainly when using rigid instruments or performing procedures such as fibroid resection.
Fluid overload, specifically with hypotonic media such as glycine or sorbitol, is a surging issue in bipolar resectoscopy. Excessive fluid absorption often leads to hyponatremia, pulmonary edema, and in severe cases, cerebral edema. Air embolism is feared during procedures where instruments are introduced without adequate cervical sealing or when excessive pressure is used during uterine distention. These risks, while statistically low, together contribute to a cautious pace of adoption in a few regions and clinical environments.
The emergence of improved distension media and advanced morcellation techniques is creating new opportunities in the field of hysteroscopy instruments by extending the scope and safety of intrauterine procedures. New instruments now favor isotonic saline, which reduces these complications. On the morcellation front, next-generation mechanical systems have made intrauterine tissue removal quick, clean, and precise. It is important in treating fibroids and Retained Products of Conception (RPOC).
Hologic’s MyoSure XL and Meditrina’s Aveta System, both launched with refined suction and blade rotation mechanisms, for example, have been widely adopted in ambulatory gynecology centers. These innovations are making hysteroscopy more accessible in fertility care. Clinics are increasingly using hysteroscopic morcellation to remove subtle intrauterine adhesions or fibroids that compromise implantation without delaying IVF cycles.
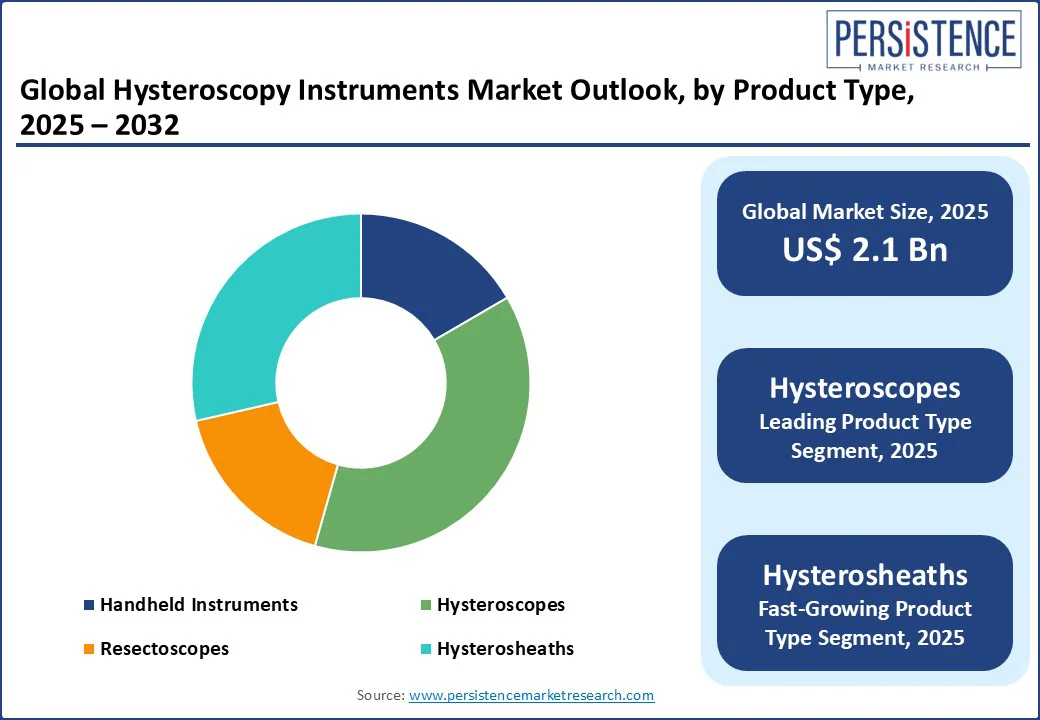
By product type, the segmentation comprises handheld instruments, hysteroscopes, resectoscopes, and hysterosheaths. Among these, hysteroscopes are speculated to hold around 37.8% share in 2025 because they serve as the primary visualization tool that makes the entire procedure possible. Their integration of optical technology, illumination, and access channels enables both diagnostic and operative tasks in the uterine cavity. The shift toward office-based hysteroscopy has further augmented demand for compact, single-use hysteroscopes.
Hysterosheaths are gaining impetus, backed by their role in enabling less invasive procedures by eliminating the requirement for cervical dilation and reducing patient discomfort. The recent surge in outpatient hysteroscopy has created high demand for small-diameter, atraumatic sheaths that promote quick and no-anesthesia procedures. Another driver is the development of double-sheath systems that allow continuous uterine distention through simultaneous inflow and outflow.
By usability, the market is bifurcated into reusable and disposable. Out of these, the disposable segment is poised to account for approximately 66.3% of the hysteroscopy instruments market share in 2025, with the ability to reduce cross-contamination risks, eliminate reprocessing delays, and improve procedural efficiency. Since the COVID-19 pandemic, infection control protocols have tightened globally, pushing several gynecology practices to move toward sterile and single-use instruments. Disposable instruments also allow gynecologists to perform see-and-treat procedures in a single visit, which is required for clinics looking to increase throughput.
Reusable hysteroscopy instruments are witnessing decent growth, backed by their long-term cost efficiency, superior performance in high-volume surgical centers, and compatibility with novel imaging systems. Large hospitals and teaching institutions continue to prefer reusable tools for their durability and versatility. Increasing adoption of bipolar resectoscopy systems with reusable electrodes, which offer better control in operative hysteroscopy, is also pushing demand.
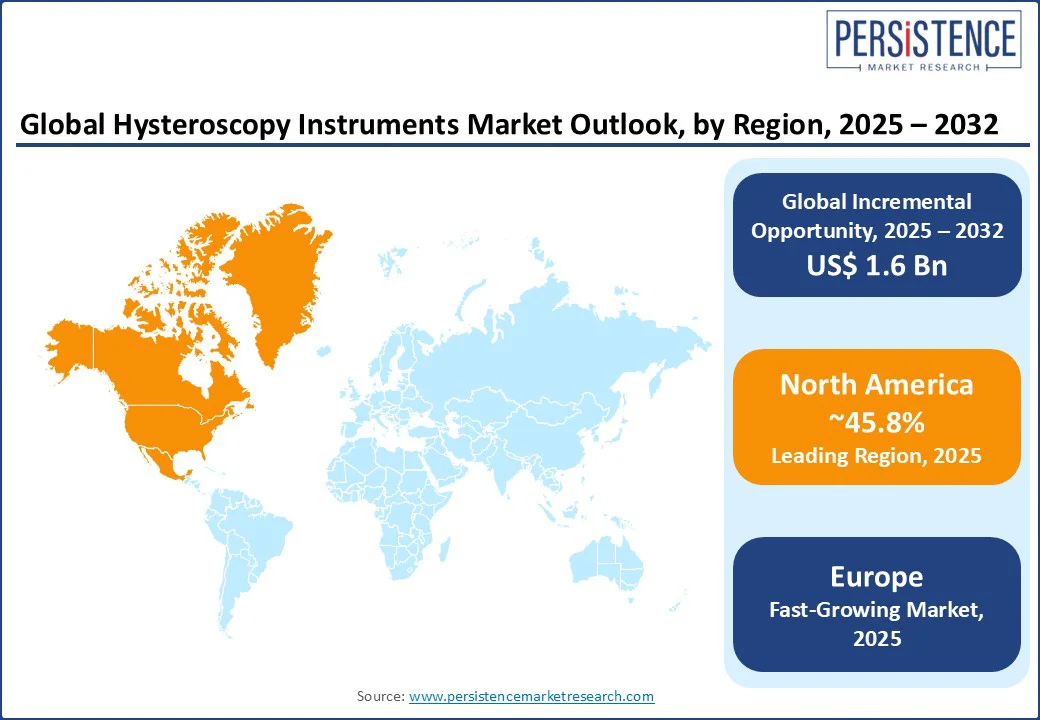
North America is predicted to account for nearly 45.8% of the share in 2025 due to a shift toward office-based and minimally invasive procedures, propelled by reimbursement changes and technological developments. The U.S. hysteroscopy instruments market is anticipated to lead with the presence of various outpatient gynecology practices and ambulatory surgical centers. The Centers for Medicare & Medicaid Services (CMS) has updated reimbursement policies that now incentivize in-office hysteroscopy.
It has led to increased adoption of portable and single-use hysteroscopic instruments, which are reducing reliance on centralized sterilization departments. Companies such as Meditrina, with its Aveta system, have targeted this demand by delivering all-in-one, disposable hysteroscopic solutions. These are being adopted by outpatient centers seeking to cut infection risks and reduce procedural overhead. Canada’s market is following a similar path with regional procurement initiatives promoting minimally invasive gynecological surgeries.
In Europe, the market is being augmented by national-level initiatives to promote day-case and outpatient gynecological procedures, primarily in Germany, the U.K., and the Netherlands. As of 2024, over 70% of diagnostic hysteroscopies in Western Europe are performed in outpatient or ambulatory settings. These are supported by reimbursement structures that favor minimally invasive approaches. The European Society for Gynecological Endoscopy (ESGE) has been a key force in encouraging the use of see-and-treat hysteroscopy models. It has accelerated demand for compact and user-friendly instruments.
Germany remains the dominant market, boosted by a well-established hospital infrastructure and widespread adoption of unique systems from local manufacturers. Richard Wolf’s Princess and Panoview hysteroscopic platforms, for instance, are widely used in local clinics for both diagnostic and operative procedures. These provide high-resolution optics and ergonomic design made for repetitive use in outpatient settings. The U.K.’s National Health Service (NHS) has also been actively investing in reducing surgical waiting times through the deployment of portable hysteroscopy units in community care settings.
Increasing awareness of minimally invasive gynecological procedures, expanding healthcare infrastructure, and a preference for fertility-related diagnostics are spurring demand in Asia Pacific. China is leading in terms of volume owing to increasing hysteroscopy procedures in the country. These are primarily supported by government initiatives in women’s health services and the surging number of outpatient departments in tertiary hospitals. Domestic players, including Mindray and Tellyes Scientific, are entering the market with competitively priced rigid hysteroscopes to challenge imported brands, further boosting accessibility.
Japan and South Korea maintain high adoption rates for reusable, precision hysteroscopes across academic and specialty hospitals. Japan-based companies are delivering high-definition hysteroscopy instruments integrated with novel fluid management and digital imaging. This shows the country’s emphasis on procedural accuracy and technology integration. In South Korea, hysteroscopy is increasingly used in IVF and Assisted Reproductive Technology (ART) clinics, complying with the country’s demographic concerns and fertility treatment demand.
The hysteroscopy instruments market houses various established medical device companies and specialized endoscopy-focused firms competing on innovation and clinical performance. Key players are dominating through extensive portfolios that include novel hysteroscopic systems with HD imaging, integrated fluid management, and modular flexibility. They are investing in research and development to improve usability and minimize patient discomfort. Small-scale players are launching simplified, cost-effective, and disposable hysteroscopic instruments aimed at extending access in outpatient and ambulatory care settings.
The hysteroscopy instruments market is projected to reach US$ 2.1 Bn in 2025.
Increasing adoption of digital hysteroscopes and surging prevalence of endometrial pathologies are the key market drivers.
The hysteroscopy instruments market is poised to witness a CAGR of 7.4% from 2025 to 2032.
Expanding outpatient infrastructure in emerging countries and strategic partnerships with OB/GYN clinics are the key market opportunities.
Karl Storz SE & Co. KG, Medtronic plc, and Richard Wolf GmbH are a few key market players.
|
Report Attribute |
Details |
|
Historical Data/Actuals |
2019 - 2024 |
|
Forecast Period |
2025 - 2032 |
|
Market Analysis |
Value: US$ Bn/Mn, Volume: As Applicable |
|
Geographical Coverage |
|
|
Segmental Coverage |
|
|
Competitive Analysis |
|
|
Report Highlights |
|
|
Customization and Pricing |
Available upon request |
By Product Type
By Usability
By Application
By End-use
By Region
Delivery Timelines
For more information on this report and its delivery timelines please get in touch with our sales team.
About Author